|
Case Series
Giant serous cystadenomas encountered in clinical practice: A case series
1 Obstetrics & Gynecology Department, Honor Health System, 19829 N 27th Ave, Phoenix, AZ 85027, USA
Address correspondence to:
Alexander Sabre
Obstetrics & Gynecology Department, Honor Health System, 19829 N 27th Ave, Phoenix, AZ 85027,
USA
Message to Corresponding Author
Article ID: 100039G06AS2024
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Sabre A. Giant serous cystadenomas encountered in clinical practice: A case series. Edorium J Gynecol Obstet 2024;9(2):10–14.ABSTRACT
Benign serous cystadenomas represent 16% of all ovarian epithelial neoplasms, and account for up to two-thirds of epithelial tumors of the ovary. They are commonly encountered after the 3rd decade of life and in the later decades, due to the slow growth nature over lifetime.
These tumors may begin as small unilocular subcentimeter lesions, but may expand to fill the entire abdominal cavity. This may present with mass effect to surrounding tissues and organs, and lead to sequela of compartment syndrome of the peritoneal cavity.
We present a case series of surgical evaluation and management of extremely enlarged serous cystadenomas of the ovary (>30 cm) encountered in an atypical age presentation, with the first case involving a 19 year old who had a known 6 cm cyst four years prior, who presented to emergency room (ER) with gastrointestinal (GI) symptoms secondary to the tumors mass effect, imaging demonstrating a massive tumor, subsequently requiring surgical dissection. The second case demonstrates a 25 year old with known cyst (>20 cm) two years prior who presented with even larger effect (close to 40 cm size) and worsening symptoms due to the tumors mass effect requiring removal. In both cases, patients presented to emergency room with acute symptoms, exploratory laparotomy was required for complete evacuation of lesion and for resolution of symptoms.
Keywords: Computed tomography, Gastrointestinal, Giant ovarian tumors, Ovarian epithelial neoplasms
INTRODUCTION
Serous cyst adenomas are benign tumors that arise from the surface epithelium of the ovary. These slow growing neoplasms may enlarge substantially due to continuous recreation of serous material into the cystic capsule and proliferation of growth factors. The mass effect of these “mammoth” tumors (>25 cm in size) may present with sequela of gastrointestinal symptoms such as abdominal bloating, constipation, cramping, and may even impact genitourinary system with symptoms such as frequency, hesitancy, and outlet obstruction [1],[2]. Abdominal compartment syndrome is a rare emergency condition characterized by the development of organ dysfunction due to increased intra-abdominal pressure. This can make initial diagnosis deferred from a primary gynecological cause to other systems.
Since these lesions arise from the adnexa, diagnosis is made with computed tomography (CT) imaging of the abdomen and pelvis and may include pelvic ultrasound to delineate ovarian parenchyma from the mass and determine blood flow [3].
We present a case series of two encounters of these severely enlarged serous cystadenomas of the ovary, diagnosed as enlarged pelvic masses on imaging, the surgical resection, and final pathological confirmation based upon histological evidence.
CASE SERIES
Case 1
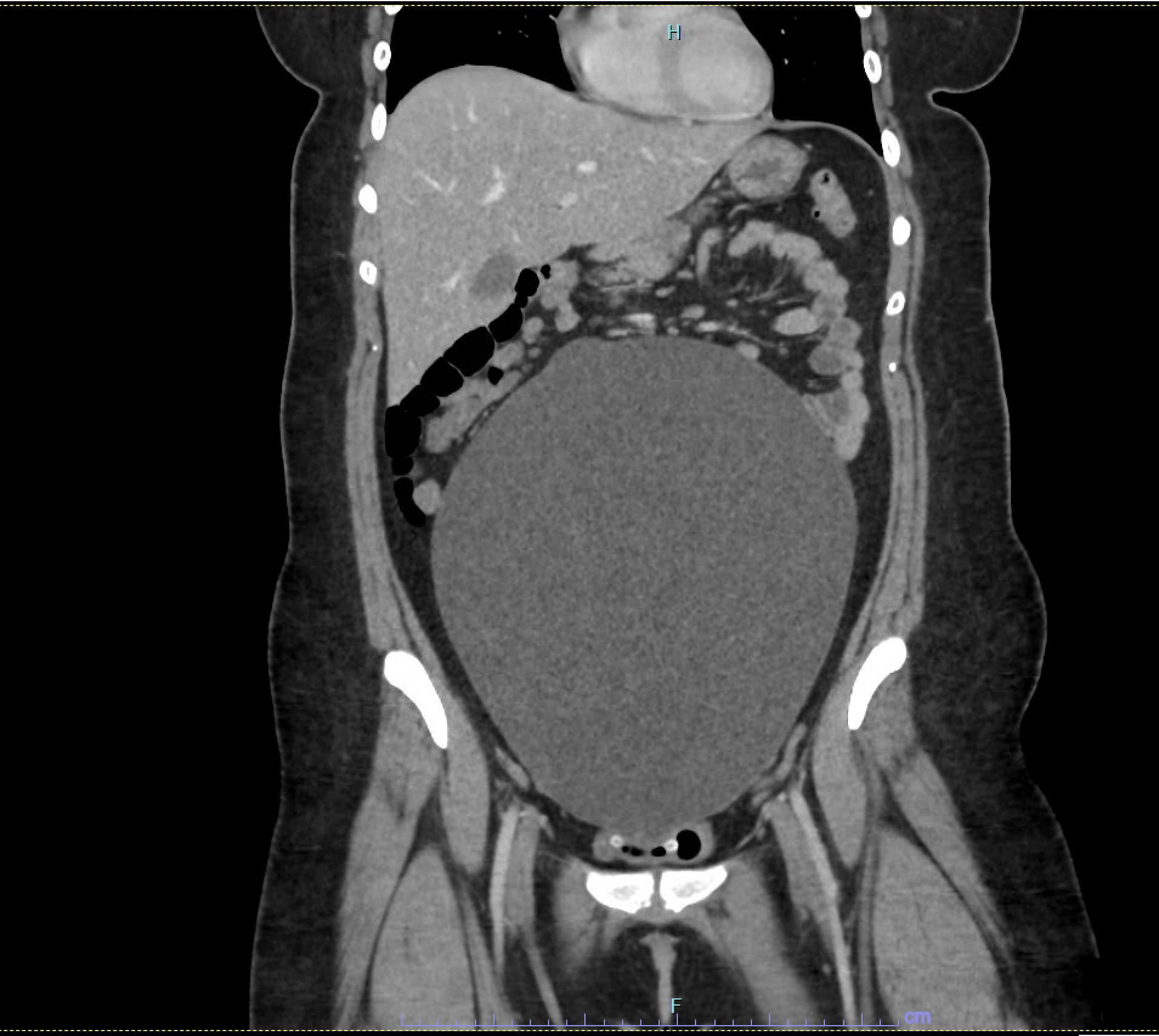
A 19-year-old gravida 0 para 0 presented to ER with worsening and waxing/waning abdominal pain with associated nausea and vomiting for two days. Past medical history significant for anovulatory menstrual cycles and chronic constipation, and a known 6.6 cm ovarian cyst four years prior. Physical exam revealed abdominal mass and generalized abdominal pain, but the patient was comfortable after 2 mg intravenous (IV) dilaudid. At that time, the patient vitals were unremarkable; Temp: 97.5F, blood pressure (BP): 139/86, Pulse: 89, respiration rate (RR): 20, oxygen saturation (SpO2): 100% on RA. Laboratory evaluation revealed the patient a mild leukocytosis of 11.8×103/uL and hemoglobin/hematocrit of 14.5 g/dL/42.1%. Abdominal/pelvic CT scan revealed a large cystic lesion in the pelvis which is likely ovarian/adnexal in origin measuring 12.5×21.7×27.6 cm (Figure 1 and Figure 2).
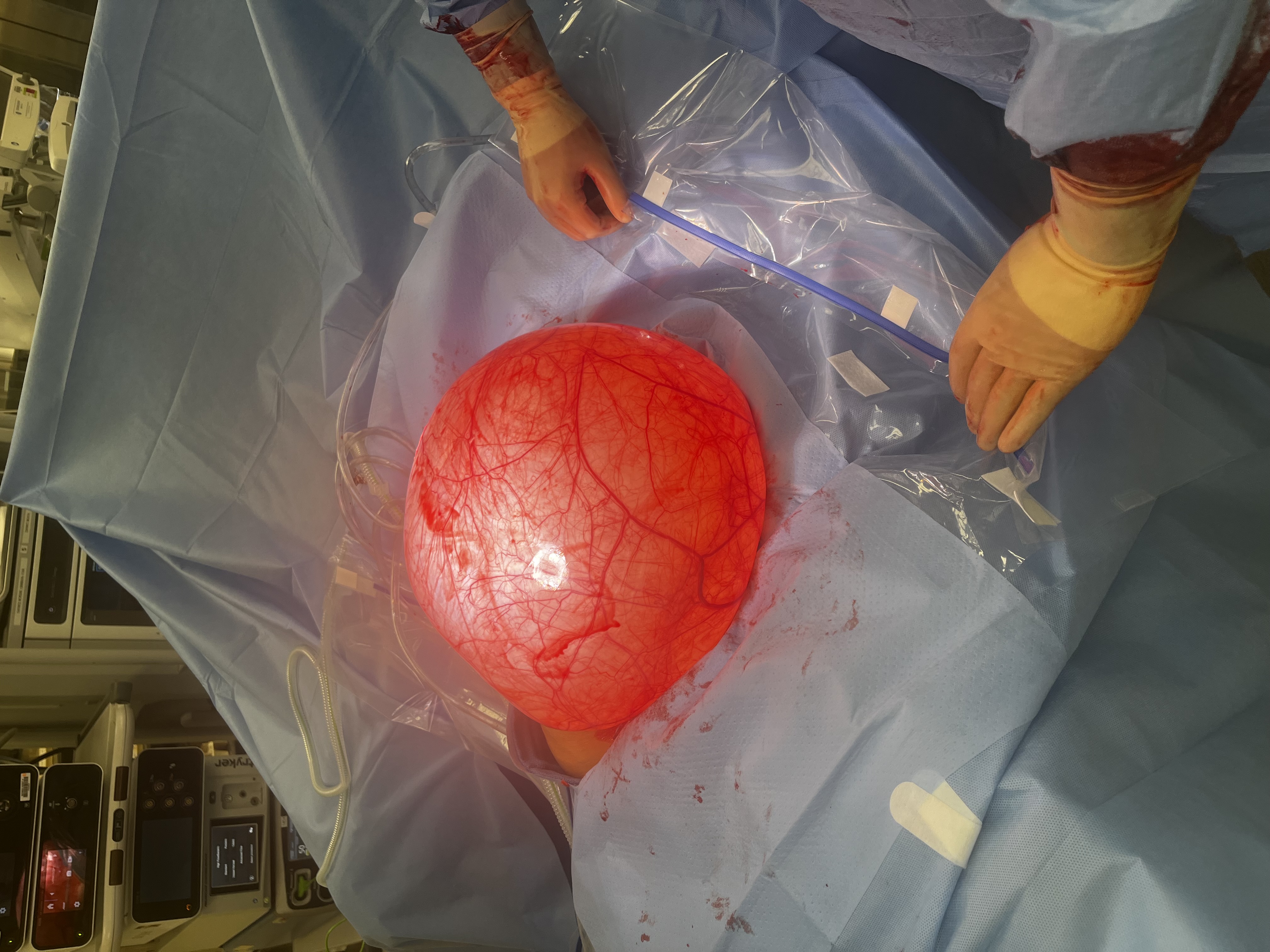
The patient was taken to operating room (OR) which revealed upon entry into peritoneal cavity a large ovarian neoplasm extending from pelvis to sub-xiphoid (Figure 3). The right ovary was distinct from the mass present on the lower portion of the infundibulopelvic ligament and was kept in situ, the right fallopian tube was indistinguishable from the whole mass. The cyst from freed from its attachments of the uteroovain pedicle and the infundibulopelvic ligament using both cautery and coagulation device and suture ligation. The cyst was taken off field without spillage of contents, transilluminated clear and weighed 10.3 lb. Blood loss was minimal to 100 mL, and the patient received 2000 mL of IV crystalloid.
The patient was discharged on post-operative day #2 upon meeting criteria (tolerating diet, resumption of bowel function, normal vitals, and lab assessment) and was seen for post-op visit two weeks later in office where dressing was removed and had an uneventful post-op course.
Case 2
A 25-year-old gravida 0 para 0 presented to emergency department (ED) with acute worsening abdominal pain and nausea and vomiting of one day duration. She reported chronic gastro-esophageal reflux disease, abdominal pain, urinary hesitancy, and constipation over past four months and stated that she had noticed distention and bloating over past four years. She had a known 20 cm cyst seen on lumbar spine imaging four years prior but did not follow-up with gynecologist and history of heavy menses. Physical exam revealed large distention of an abdominal mass up to the xiphoid process along with generalized abdominal pain. At that time, the patient vitals were unremarkable; Temp: 98.4F, BP: 136/98, Pulse: 75, RR: 18, SpO2: 98% on RA. Laboratory evaluation was unremarkable. Abdominal/pelvic CT scan revealed a massive hypodense cystic lesion occupying the entire abdomen and pelvis measuring 2734×36 cm (Figure 4 and Figure 5).
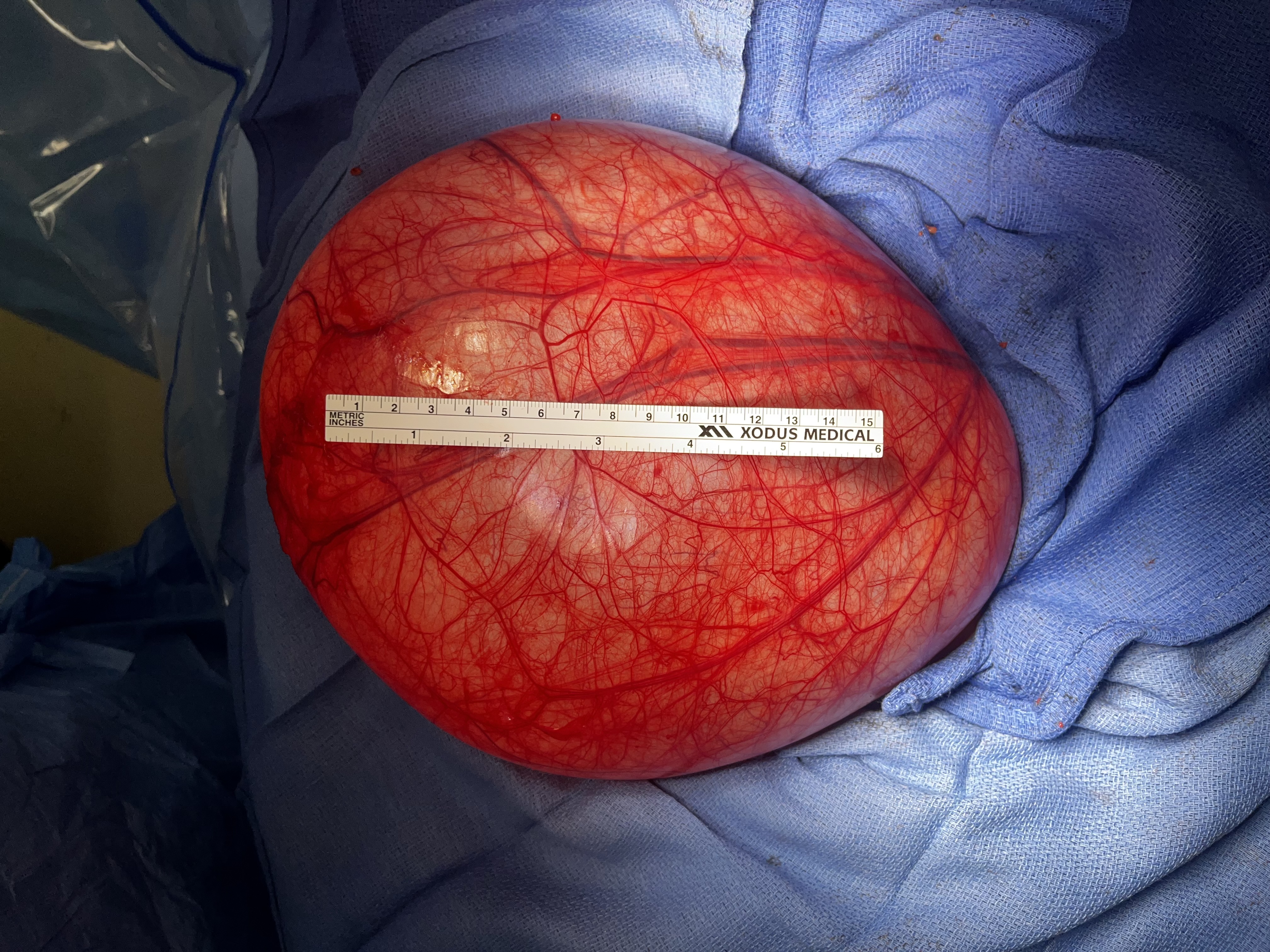
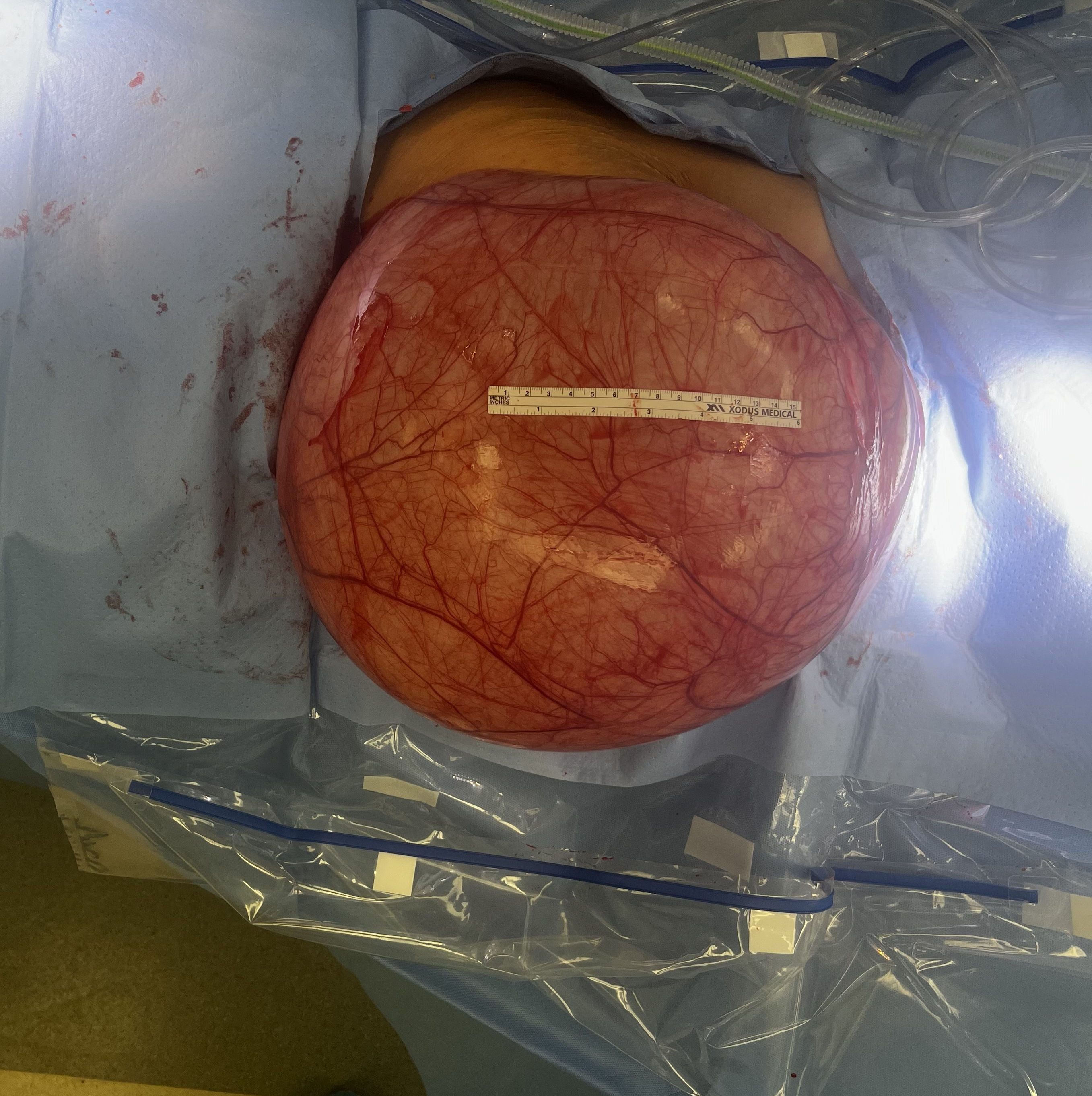
The patient was taken to OR, which revealed upon entry into peritoneal cavity the couple replacement with a large simple unilocular cyst involving the fallopian tube and right ovary (Figures 6, Figure 7, Figure 8). The patient’s bowel was displaced cephalad from the mass effect of cyst. The right ovary was attached to the cyst and the sheer distortion of anatomy and blood vessels of the infundipulopelvic ligament did not make preservation possible. As well the right fallopian tube was indistinguishable from the whole mass. The cyst from freed from its attachments of the uteroovain pedicle and the infundibulopelvic ligament using both cautery and coagulation device and suture ligation. The cyst was taken off field without spillage of contents, transilluminated clear and weighed 35.3 lb. Blood loss was minimal to 150 mL and patient received 1500 mL of IV crystalloid.
The patient was discharged on post-operative day #2 upon meeting criteria (tolerating diet, resumption of bowel function, normal vitals, and lab assessment) and was seen for post-op visit two weeks later in office with resolution of genitourinary and gastrointestinal chronic complaints.
DISCUSSION
Ovarian serous cystadenoma arises from the surface epithelium of the ovary. They are usually unilocular oval shaped with a glistening surface and filled with either clear or yellow-tinged cystic fluid; they are commonly about 3–10 cm in diameter, but may rarely grow to sizes >30 cm in diameter. Histopathology reveals they have a single layer of ciliated simple columnar or simple cuboidal non-ciliated epithelium which is comparable to tissue of the fallopian tube [4]. This connection may be a reason for involvement of surroundings structures, and not only the ovarian tissue, as was encountered in our first case, where the ovary was distinct from the cystic lesion.
Giant ovarian tumors may initially present in patients as an asymptomatic increase in abdominal girth, or may be accompanied by symptoms of nausea, vomiting, increased urinary frequency, urinary retention, constipation, and dyspnea due to the neoplasms mass effect on surrounding viscera [5]. Dysmenorrhea is also a common symptom which occurs in patients effected with epithelial tumors of the ovary [6]. These symptoms were present in both cases, highlighting the need for clinicians to have high suspicion when encountering gynecological neoplasms.
The mass effect of these extremely large tumors causes intra-abdominal hypertension that are manifested with pathophysiologic symptoms in cardiovascular, pulmonary, and gastrointestinal systems. This can be characterized as an elevated diaphragm, a reduction in compliance of the lung, chest, and abdominal wall, cause diminished venous return and celiac blood flow [7].
Removing the giant ovarian cyst may also be associated with the risk of intra- and post-operative morbidity. Factors that influence this morbidity are duration of operation, technically difficult surgery, excessive blood loss, and sudden reduction of the chronic increase in intra-abdominal pressure. After sudden abdominal decompression, there is a potential risk of cardiorespiratory collapse due to the paradoxical movement of the thinned diaphragm, and changes in abdominal vascular tone, which cause altered mechanics of ventilation and circulation leading to life-threatening pulmonary edema [8]. Patients with masses occupying the entire abdominal cavity require careful intra-operative fluid management, and careful surgical technique are key factors to decrease complications. Post-operatively, reducing ileus, providing adequate respiratory support, supporting abdominal wall tension, and monitoring hemodynamic parameters are important guidelines to recovery [9]. There may be cosmetic defects after removal of such large masses. Abdominal wall reconstruction might be necessary because of the laxity and redundancy of the skin [10]. Fortunately, in the presented case series, both surgical removals of these giant ovarian neoplasms had uneventful postoperative periods and did not require subsequent surgical reconstruction, likely due to no underlying medical issues and each patients young age.
CONCLUSION
This case series reviews the successful surgical evaluation and management of extremely enlarged serous cystadenomas of the ovary encountered in atypical age presentations. Careful surgical evacuation, intra-operative management, and post-operative management prevented complications which may arise due to the characteristics of these mammoth neoplasms.
REFERENCES
1.
Novakov I, Timonov P, Fasova A. Mammoth bilateral ovarian serous cyst adenomas in a postmenopausal woman: A rare case report. Cureus 2023;15(11):e48935. [CrossRef]
[Pubmed]

2.
Khormi GJ, Ageeli RS, Othathi RJ, Bingasem SM, Al Ghadeeb M. Abdominal compartment syndrome due to large ovarian cystadenoma: A case report. Cureus 2022;14(11):e31389. [CrossRef]
[Pubmed]

3.
Deligeoroglou E, Eleftheriades M, Shiadoes V, et al. Ovarian masses during adolescence: Clinical, ultrasonographic and pathologic findings, serum tumor markers and endocrinological profile. Gynecol Endocrinol 2004;19(1):1–8. [CrossRef]
[Pubmed]

4.
Mounir B, Anas E, Yassine E, et al. Incidental discovery of a giant ovarian cystadenoma. Ann Med Surg (Lond) 2022;82:104698. [CrossRef]
[Pubmed]

5.
Schultz KAP, Sencer SF, Messinger Y, Neglia JP, Steiner ME. Pediatric ovarian tumors: A review of 67 cases. Pediatr Blood Cancer 2005;44(2):167–73. [CrossRef]
[Pubmed]

6.
Tsai JY, Saigo PE, Brown C, La Quaglia MP. Diagnosis, pathology, staging, treatment, and outcome of epithelial ovarian neoplasia in patients age < 21 years. Cancer 2001;91(11):2065–70. [CrossRef]
[Pubmed]

7.
Cheatham ML. Abdominal compartment syndrome: Pathophysiology and definitions. Scand J Trauma Resusc Emerg Med 2009;17:10. [CrossRef]
[Pubmed]

8.
Sheldon R, Eckert M. Surgical critical care: Gastrointestinal complications. Surg Clin North Am 2017;97(6):1425–47. [CrossRef]
[Pubmed]

9.
Pilone V, Tramontano S, Picarelli P, et al. Giant mucinous ovarian borderline tumor. A good lesson from an asymptomatic case. Int J Surg Case Rep 2018;50:25–7. [CrossRef]
[Pubmed]

10.
Hackethal A, Brueggmann D, Turovets M, et al. Removal of enormous bilateral mucinous cystadenomas of the ovaries with abdominal plastic reconstruction. Arch Gynecol Obstet 2009;279(1):65–7. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Alexander Sabre - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthor declares no conflict of interest.
Copyright© 2024 Alexander Sabre. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.